Complex PTSD (CPTSD) and borderline personality disorder share some common symptoms and can coexist.
The symptoms of complex post-traumatic stress disorder (CPTSD) and borderline personality disorder (BPD) are similar.
But there are key differences in emotional regulation and troubled relationships that set CPTSD and BPD apart.
Knowing the differences can help people with either condition better understand themselves and get the right treatment. BPD and CPTSD are treatable, even if they occur together.
Complex PTSD (CPTSD) is a subtype of post-traumatic stress disorder (PTSD).
CPTSD isn’t currently recognized in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, text revision (DSM-5-TR) as a separate disorder from PTSD.
But the International Classification of Diseases, 11th edition (ICD-11), used by the World Health Organization (WHO) and many clinicians, considers CPTSD a different category of PTSD.
CPTSD includes all the symptoms of PTSD plus additional symptoms that include a negative self-image, difficulty regulating emotions, and problems with interpersonal relationships
This condition is typically seen in someone who’s experienced chronic or repeated trauma, such as survivors of prolonged childhood abuse and refugees. But a single traumatic event can also cause CPTSD.
Signs and symptoms of CPTSD
The signs and symptoms of CPTSD include the three categories of PTSD symptoms:
- Intrusive thoughts: Intrusive thoughts can include recurring memories, flashbacks, nightmares, and emotional or physical reactions to reminders of the traumatic event.
- Avoidance behaviors: People often avoid places or situations that remind them of a traumatic event. They may also avoid talking about anything related to the trauma.
- Increased arousal: Sleep problems, irritability, heightened anger or anxiety, and difficulty concentrating are a few common arousal symptoms.
The symptoms are often strong and frequent and are primarily related to the initial traumatic event. CPTSD presents additional symptoms such as:
- Emotional dysregulation: This is the inability to manage the duration and intensity of negative emotions. This may also include dissociation and disconnection from those around you.
- Negative self-view: Shame or guilt are more common with CPTSD than PTSD. With CPTSD, you may feel the traumatic events were your fault or caused by a defect in yourself. These emotions can lead to depression and suicidal thoughts.
- Difficulty in personal relationships: Trust is difficult for people with CPTSD because they tend to feel that people will inevitably hurt them.
- Loss of belief system: Your worldview or religious beliefs change.
Borderline personality disorder (BPD) affects a person’s ability to regulate their emotions.
The lack of self-regulation can lead to impulsivity and difficulty in personal relationships and affect how the person sees and feels about themselves.
Frequent changes in mood and extreme changes in point of view are common symptoms, as well as turbulent feelings about oneself and relationships with others.
BPD is more common among people who’ve experienced traumatic life experiences such as abuse and abandonment.
Signs and symptoms of BPD
To those around them, the feelings of a person with BPD can change quickly and without warning. They may also:
- view the world in extremes
- quickly change values or worldviews
- have difficulty with impulse control
- have impulsive behaviors, such as unsafe sexual intercourse, reckless driving, and spending sprees
- fear abandonment and go to extremes to prevent real or perceived abandonment
- experience intense, inappropriate anger
- have suicidal thoughts and behavior
- have a chronic sense of emptiness
- experience dissociation
Suicide prevention
CPTSD and BPD may increase your chance of self-harm. If you’re considering self-harm or suicide, you’re not alone. Help is available right now. You can:
- Call a crisis hotline, such as the National Suicide Prevention Lifeline at 800-273-8255.
- Text HOME to the Crisis Text Line at 741741.
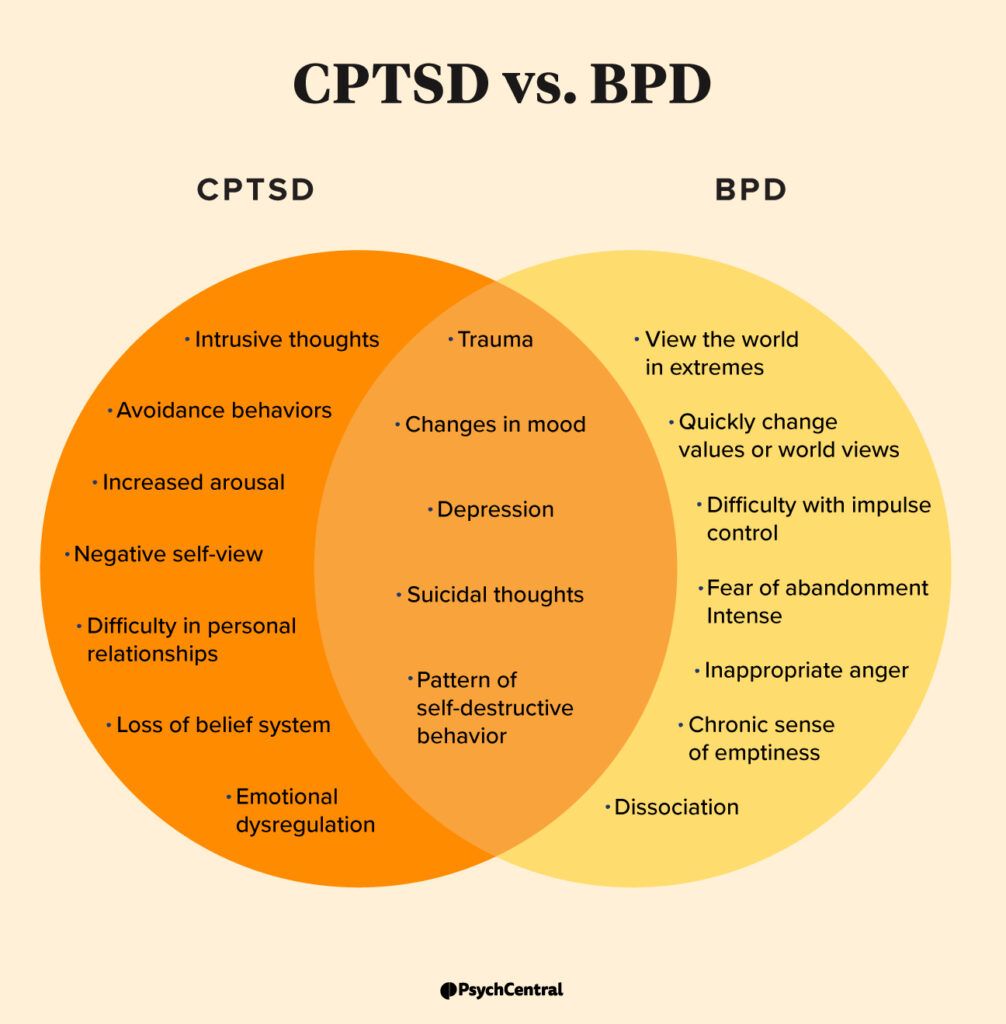
Both disorders share some similarities and differences. CPTSD and BPD both can stem from trauma. They both can cause mood changes, depression, and suicidal thoughts. People with these conditions can also develop a pattern of self-destructive behavior.
In the past, mental health professionals have contemplated classifying CPTSD as a replacement diagnosis for BPD and other times as a subtype of BPD, according to
But a
Where these disorders tend to differ is in emotional regulation and the nature of the relationship problems people with these conditions experience.
With CPTSD, emotional dysregulation revolves around a person’s inability to calm themself down. But with BPD, emotional regulation tends to involve uncontrolled anger and more severe emotional disturbances.
People with CPTSD and people with BPD can also show difficulties in personal relationships, but there are differences.
A person with BPD may go to extreme lengths to avoid real or perceived abandonment, with many of the relationship issues stemming from this behavior. A person with CPTSD may have issues with trust and staying connected with people, but they don’t have the fear of abandonment; that’s a telltale sign of BPD.
Yes, you can have CPTSD and BPD together.
There’s also evidence that the two are more likely to be connected when the initial trauma stems from physical neglect and emotional abuse.
CPTSD and BPD can occur separately or together and are usually caused by a traumatic event or a history of prolonged trauma.
Mental health professionals can help relieve symptoms through therapy or a combination of medication and therapy.
The most common therapy used is dialectical behavioral therapy (DBT). First developed to treat BPD alone, DBT teaches you to live in the moment and be aware of emotions and helps you establish healthy relationships.
You can learn more about it and try a few exercises at dialecticbehavioraltherapy.com.
Taking steps to care for your mental health can help you manage both symptoms and improve your mental well-being.
If you’re unsure where to start, you can check out Psych Central’s guide to finding mental health support.
