Can your gut health cause or worsen depression? Emerging research says that mental health and gut biology are more closely linked than you might think.
An upset stomach can definitely make you feel terrible, but can your gut health really influence your mental condition?
Your gut and brain are intrinsically linked. Think about a time when you felt anxious about something: You probably experienced some kind of literal gut feeling, like nausea or butterflies.
If the gut and brain are connected, does that mean that treating gut issues can cure mental health conditions like anxiety and depression?
There’s still work to be done in terms of researching gut-specific treatments for mental health conditions, but the known link between the brain and gut suggests a promising avenue for mental health treatment.
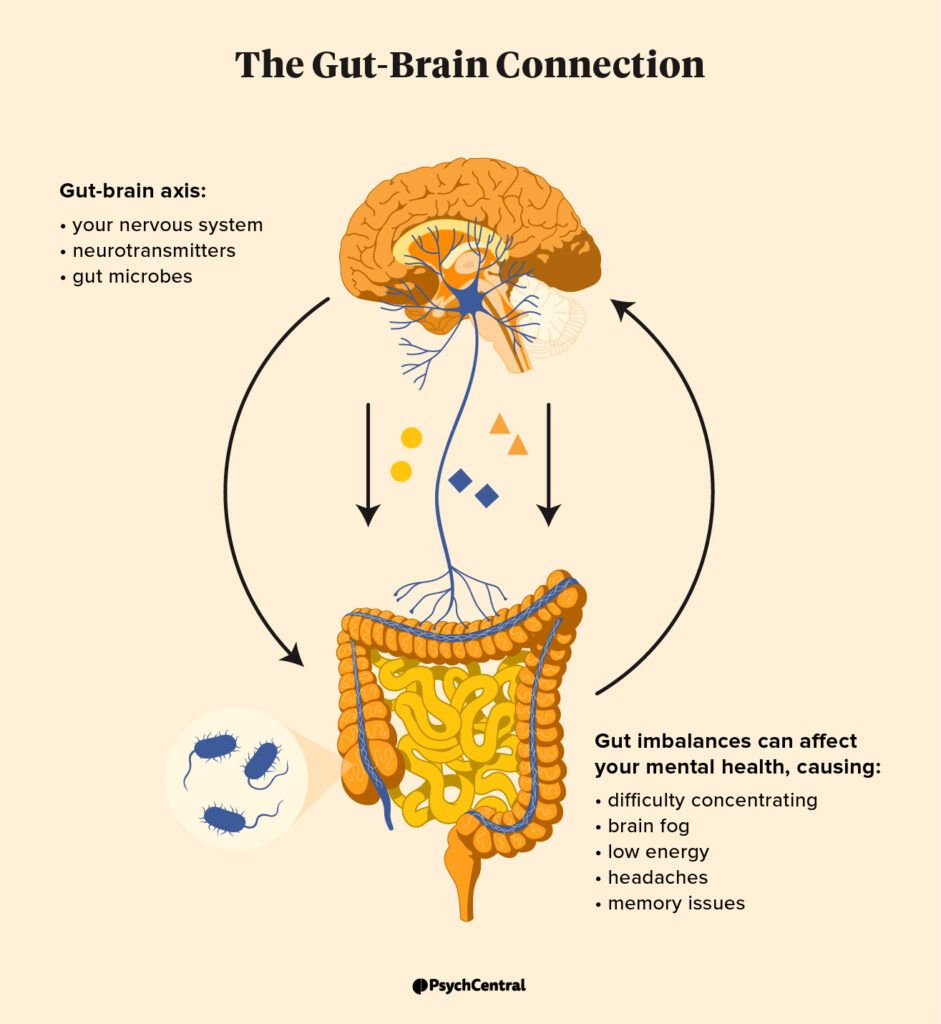
The gut-brain connection, also known as the gut-brain axis (GBA), involves:
- your nervous system
- neurotransmitters
- gut microbes and chemicals
“All of the body’s commands come from neurons, which can be found in the brain and the gut,” says gut health expert Mahmud Kara, MD.
Neurotransmitters, including serotonin, play a crucial role in regulating mood. “Interestingly, 80% of serotonin is produced by the gut,” explains Kara. Your gut also contains trillions of microbes that make up its microbiome.
Neurons in your gut’s microbiome don’t just impact your gut health. They interact with other parts of your body, too — like your brain. Kara gives the example of short-chain fatty acids (SCFAs). The gut produces SCFAs, which then go on to promote memory formation in the brain.
So how does the gut-brain connection relate to mental health?
A good real-world example of how this connection works is when you feel anxious.
“When anxiety hits, your body is bombarded with [neurotransmitters] — it’s part of the fight-or-flight response that has protected us for centuries. This can lead to physical symptoms that are often associated with anxiety, such as diarrhea, nausea, or abdominal discomfort,” he explains.
This is a solid example of the brain impacting the gut. But what about the other way around? According to Kara, poor gut health or bacterial imbalances in the gut microbiome can also impact the brain.
“An imbalance in the gut microbiome can disrupt the typical production of hormones and neurotransmitters that impact our mood and state of mind,” he adds.
According to Kara, imbalances may also lead to chronic inflammation over time, which has been linked to conditions like Alzheimer’s disease. Gut imbalances may also negatively affect neurotransmitter production, potentially playing a role in depression.
“On the flip side, this same gut-brain axis can work in our favor,” Kara says. Improving digestive health can then lead to improvement in overall health, including mental health, he adds.
Leaky gut
Leaky gut, which happens when there’s damage to the lining of your gut wall, may make you more vulnerable to harmful substances, says Kara.
This can lead to health issues like:
- digestive troubles
- brain fog
- fatigue
- headaches
- skin changes
If your gut wall is compromised, this can also disrupt your gut’s microbiome. This impacts hormone and neurotransmitter production, which may affect your nervous system and mental health, explains Kara.
It’s important to note that not all health experts consider leaky gut syndrome to be an actual condition. The Canadian Digestive Health Foundation (CDHF), for instance, explains that gut permeability may be a symptom of some digestive conditions but isn’t a cause for them.
“Some of the physical symptoms that are associated with anxiety and depression can also be linked to poor gut health,” says Kara. These may include:
- diarrhea and constipation
- nausea
- bloating
- abdominal discomfort
Kara also points out that poor gut health can cause symptoms usually associated with mental health conditions like:
- difficulty concentrating
- brain fog
- low energy
- headaches
- memory issues
One systematic review and meta-analysis from 2017 found that people with irritable bowel syndrome (IBS) had higher levels of depression than people without IBS.
According to Kara, other digestive disorders like celiac disease and Crohn’s disease can also disrupt the gut microbiome and cause cognitive symptoms.
It’s important to talk with a doctor and get a proper diagnosis for digestive health conditions, since some can worsen without treatment and cause permanent damage. Additionally, getting help for a gut health problem may help reduce mental health condition symptoms.
The first-line treatment for depression typically involves a combination of medication, therapy, and lifestyle changes. Emerging evidence also suggests that promoting a healthy gut flora may help with certain mental health conditions.
For example, one
A
But in both cases, researchers note that further study is needed to determine a safe and effective gut-specific treatment for mental health conditions like depression.
There’s still no scientifically proven probiotic or gut treatment remedy for depression or anxiety.
That said, we do know that things like probiotics, prebiotics, and postbiotics can help improve gut health, says Kara, which may, in turn, improve mental health:
- Probiotics. Probiotic foods include kefir, yogurt, kimchi, tempeh, and other fermented foods. You can also consume probiotics in supplement form.
- Prebiotics. Prebiotics are a form of dietary fiber and can be found in chicory root, garlic, onions, leeks, and more.
- Postbiotics. Postbiotics are bioactive compounds created when the gut ferments fiber. You can buy these in supplement form at some health food retailers.
While consuming probiotics may not necessarily cure your depression, research suggests improving gut health may be a promising option for relieving depression symptoms.
There’s no FDA-approved depression treatment targeting gut health. Still, you might find it helpful to work on balancing your gut’s microbiome.
Things you can do to improve your gut health include:
- eat more probiotic foods
- take probiotics
- include prebiotic fiber in your diet
- reduce your sugar consumption
- limit stress
- avoid taking antibiotics unnecessarily
- exercise regularly
- get quality sleep
- consider cutting down or quitting smoking
Note that probiotics and prebiotic supplements can have side effects. And, if your digestive symptoms are severe, you may want to consider seeing a gastroenterologist.
Similarly, if your depression symptoms impact your ability to function day-to-day, you may find it helpful to reach out to a mental health professional.
